The NHS 10 Year Health Plan and the Life Sciences Sector strategy set out a vision for the NHS to be transformed, digitally enabled and a driver of innovation. Recent announcements and publications shed new light on the evolving structure of the NHS but many questions still remain. The extent of the change and the number of publications are dizzying: the abolition of NHS England, reforms to Integrated Care Boards (ICBs) and regional restructuring are set up to transform the NHS. The emerging NHS will look very different, with new responsibilities, different incentives and very critical digital agenda.
Key Features of the New NHS Structure:
- DHSC HQ:
- Sets national strategy, priorities, allocates funding, and manages national performance.
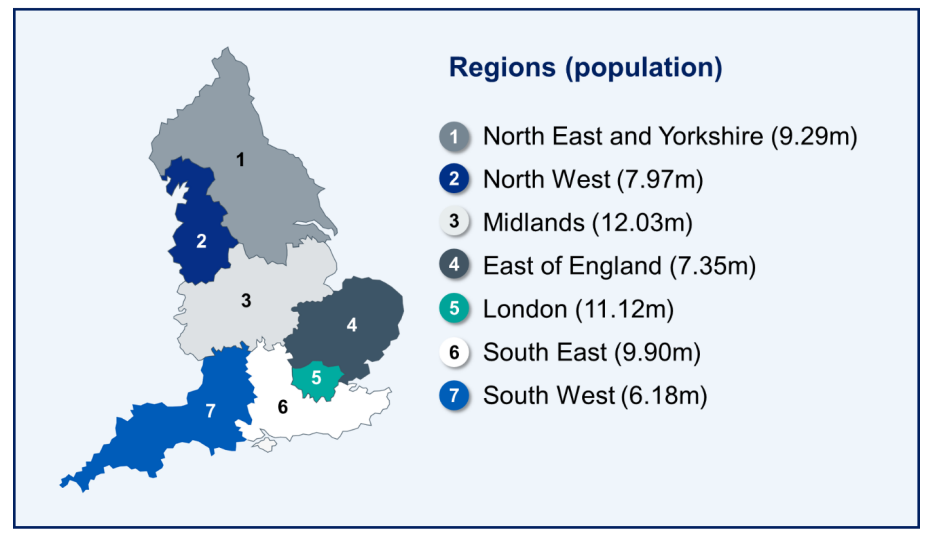
- DHSC Regions:
- Seven regions, each responsible for regional strategy and Integrated Care Board capability development. Regions monitor and support underperforming services and lead improvement initiatives.
- Regional Leadership: Region CEOs are accountable to ICB and provider CEOs, while Region Chairs oversee non-executive directors.
- Integrated Care Boards:
- Shift to outcomes-based commissioning aimed at improving population health and reducing inequalities.
- The number of ICBs will reduce from 42 to 26 clusters, with a focus on building Neighbourhood Health Services.
- Providers:
- NHS organisations remain the frontline delivering high-quality care.
The Data and Digital Core
An increased emphasis on data, digital, and analytical capabilities drive the new NHS structures and what they will be able to do. ICBs are tasked with developing and using linked, individual-level datasets, service usage statistics, and outcomes data. This data should create real-time dashboards so services can be monitored in real time and service demand can be predicted. The intention is that this insight will inform commissioning, allowing ICBs to introduce new providers where needed and plan for the changing needs of the population.
It’s good to see there’s not a reliance on just the data, after all datasets are often imperfect and incomplete giving just partial insight. ICBs must therefore build strong community engagement, ensuring that the data insights are robustly tested and enriched by local voices.
Significant questions persist: Can data-sharing agreements be established swiftly enough to enable linked datasets? Is the quality and availability of outcomes and usage data good enough to get started? Do we have the workforce with the right skills, and is there a clear understanding of gaps? Most critically, do ICBs have the partnerships and expertise required to reach marginalised and excluded groups?
People, Skills and Leadership
The success of these changes hinges on people – their skills, knowledge, confidence, numbers and leadership. In the newly emerging NHS model the workforce responsibilities are shared between DHSC Regions and NHS providers. Regions are expected to plan workforce and their professional development to have the workforce and skills to use the data and work in communities as well as deliver services. Providers are responsible for their workforce planning and development.
DHSC Regions also oversee leadership development. Leadership has been an enabler and barrier for innovation and digital transformation in the NHS. For the vision of the NHS 10 Year Plan to be successful DHSC Regions will need to be able to support and equip leaders to drive digital transformation and innovation. Can they do this in a way that builds the necessary workforce without fuelling competition for scarce digital talent?

Setting Up A New Era for Research and Innovation
DHSC Regions are intended to become drivers of research and innovation ensuring digital transformation aligns to the 10 Year Health Plan. This starts with a responsibility to develop digital strategies for the geographical patch and act as a hub for digital expertise for the region. They also will oversee ICB and provider research performance and delivery, the Health Innovation Networks and the use of research (NIHR) capabilities. But there are also new responsibilities and expectations so they can be an enabler of NHS innovation and research.
The 10 Year Health Plan introduced two new NHS innovation capabilities - Regional Health Innovation Zones and Integrated Health Organisations (IHOs). These zones are intended to create collaborations and partnerships between NHS, mayors, academia and industry to experiment, test and generate evidence in order to redesign pathways. Integrated Health Organisations are Foundation Trusts that meet a core set of standards which then open new opportunities and capabilities. This includes keeping savings to reinvest in new projects, developing innovative transformation initiatives and providing startup support. Regions are expected to identify potential Trusts to become IHOs and support their development.
However, scaling innovation remains a perennial challenge. Should regions adopt a single digital tool for consistency and supplier benefit, or allow local leaders the flexibility to choose, fostering variety but risking fragmentation? Should suppliers be concerned if whole region scaling means only 7 opportunities to enter the NHS? And what about primary care innovation?
Summary
The recent changes to the NHS introduce new structures and incentives that put data, digital, and community engagement at the centre of decision making but it’s unclear what the balance of these will be. The success of the new NHS model depends on overcoming challenges around data sharing, workforce capability, and the adoption of digital tools – longstanding challenges! At the same time, the NHS must become more adept at research and innovation with DHSC Regions expected to enable this. The risk is if scale is pursued at the expense of variety, suppliers may be limited to just seven regional opportunities, potentially stifling innovation and aspiration of the NHS to support economic growth. Presumably primary care innovation is synonymous with Neighbourhood Health Service aspirations, which is a potential limitation. The recent changes means the NHS has new opportunities to develop innovations that work for patients and staff making the 10 Year Plan a reality.
I hope you enjoyed this post, if so please share with others and subscribe to receive posts directly via email.
Get in touch via Bluesky or LinkedIn.
Transparency on AI use: GenAI tools have been used to help draft and edit this publication and create the images. But all content, including validation, has been by the author.