It’s two weeks since the much-anticipated NHS 10-year plan was unveiled. But despite its title (and as many have commented) the document feels less like a “plan” and more like a “vision.” Why? Because a core component you might expect in a plan is missing: a delivery chapter.
The omission hasn’t gone unnoticed. Many have pointed out that without a delivery plan, it risks becoming just another document full of aspirations. There have been rumours a delivery chapter exists and suggestions it may still see the light of day. But its absence raises important questions about how change is expected to happen at scale.
It’s not that the vision lacks merit. It touches on key themes and technologies like digital transformation, virtual wards and AI. But without detail on how to deliver that transformation, it falls short of being actionable. It’s a vision that forgets about the foundations of technology infrastructure and the experiential aspects of healthcare, such as how patients and clinicians interact with technology. Successful digital change means designing tools that are so intuitive, so seamless, that they become invisible and the application feels obvious.
Perhaps what is most disappointing is that we don’t lack for good ideas, we lack delivery and implementation. The NHS has no shortage of national strategies or well-intentioned roadmaps. What’s been missing is successful implementation at scale.
To be fair, there are pockets of incredible innovation and implementation across the system. Implementation is happening just not consistently, and not nationally. For example, 6% of NHS hospitals are yet to deploy electronic health records. Virtual ward uptake varies wildly, and patient access to medical records remains widely variable even within very small areas. This variation has emerged despite past national strategies with delivery plans.

Opportunity to break from the past
Historically, national programmes have leaned heavily on long, one-size-fits-all type guidance documents. There have been blueprints and playbooks for numerous transformation programmes attempting to capture and generalise unique journeys in increasingly more documentation. But real-world change isn’t linear. It depends on local context, technology stacks, workforce capabilities, demographic needs, and leadership culture which all vary widely. What works in one region may not work in another. And pretending otherwise gets us to where we are now.
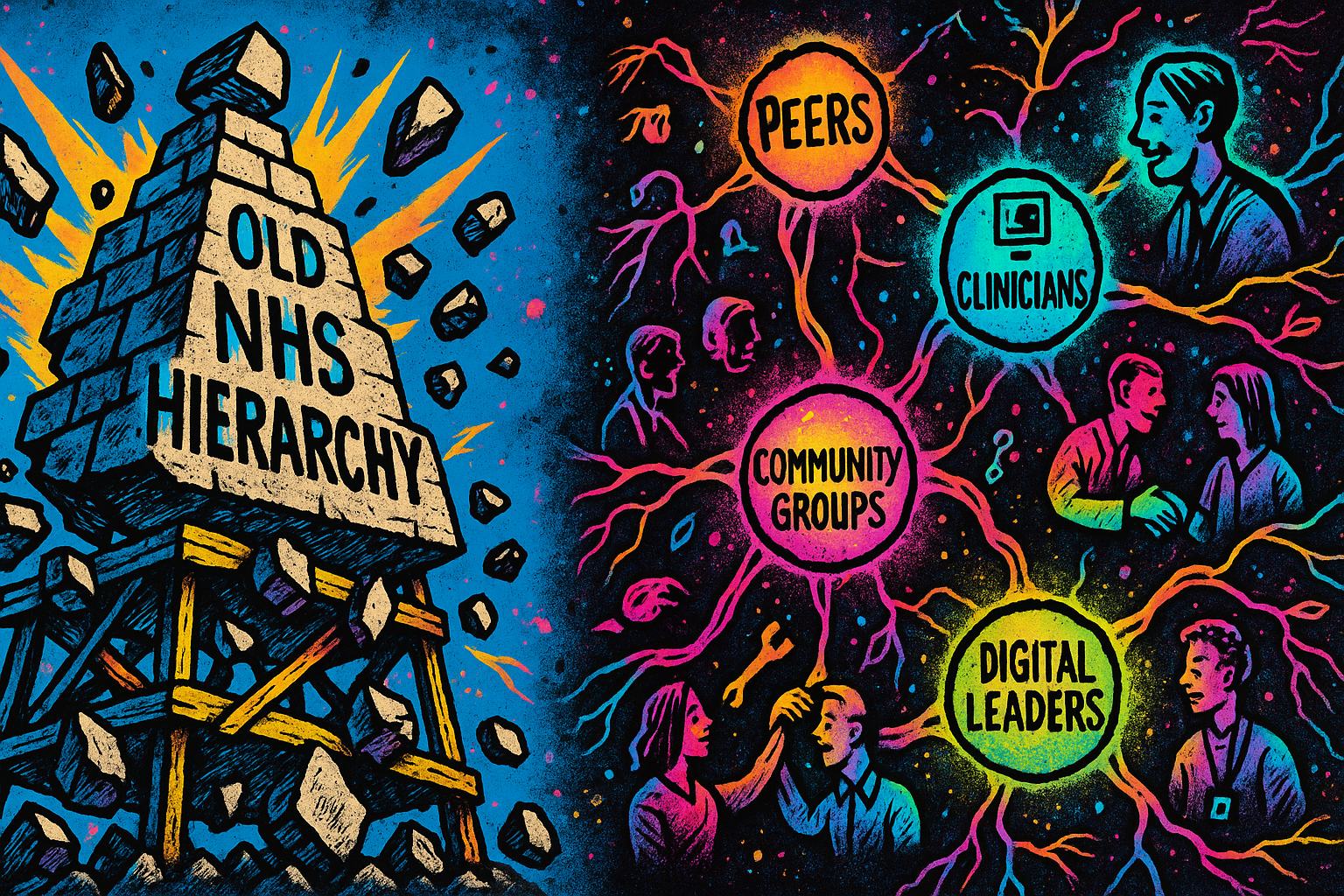
So perhaps we should welcome the fact that the delivery chapter is missing. Maybe it’s time to recognise the previous approaches to transformation have much room for improvement. In which case the challenge of a missing delivery chapter is also an opportunity: for local leaders, digital champions, clinicians, digital teams, and partners to step into the vacuum and deliver transformation from the ground up in a way that works for them and their communities.
What is needed to have locally driven transformation?
1. Local leadership that is willing to step into the vacuum to convene partners across NHS, local authorities, social care, communities, industry and research in order to create the coalition to plan, develop and test solutions.
2. Communities of practice and knowledge exchange supported by leaders who protect staff time along with national funding and support for peer networks, scholarships, placements, mentoring and shadowing. We need these communities to lead the creation of templates and material for shared learning that are practical, not prescriptive.
3. And there is a need for a central support structure that includes not just policy guidance but timely funding announcements with ample notice, transparent criteria of success, and support to build local capability. This support must include investment in digital skills and training. It must empower organisations to assess their own technology stack, understand what’s missing, and plan strategically with industry partners. And crucially, it must celebrate and elevate those who are already delivering change, pushing boundaries, trying new models, and improving services. Celebration helps to normalise bottom up driven delivery of change with people and communities.
The NHS has an opportunity to shift from hierarchy to networks and from blueprints to lived experience. The absence of a delivery chapter could be a quagmire of indecision or it could be a catalyst for a different approach to transformation. Past delivery approaches have had mixed success so perhaps it's time to do things differently.
You made it to the end!
Hopefully that means you enjoyed this post, if so please share with others and subscribe to receive posts directly via email.
Get in touch via Bluesky or LinkedIn.
Transparency on AI use: GenAI tools have been used to help draft and edit this publication and create the images. But all content, including validation, has been by the author.