Healthcare systems, like the NHS, use market forces to bring new products and services into the system at scale by creating marketplaces using procurement frameworks. The theory is creating a marketplace means solution providers compete for customers which results in better solutions for healthcare organisations which are quality assured and at competitive prices. The solution provider benefits from the market by being able to scale the solution reducing costs and increasing revenue. At a first glance this would appear to be a win-win, a route to benefit both NHS and solution providers. In taking this approach where we have a marketplace for complete solutions that can 'drop in' to healthcare systems are we in reality creating more inefficiencies and is there a better way?
The flexible healthcare organisation
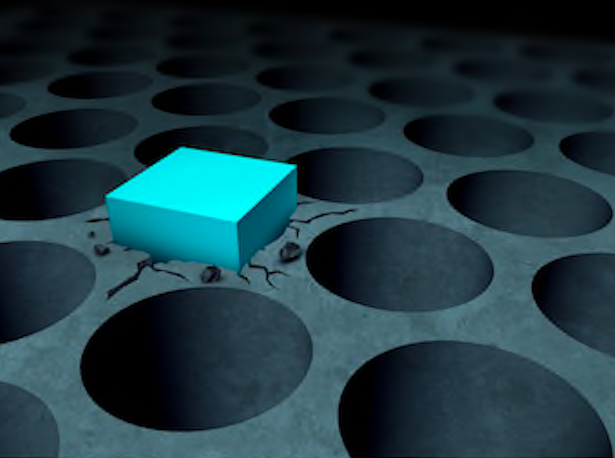
New solutions are commissioned through frameworks outlining the requirements and functionality creating the markets. Solution providers meet this minimum set of functionalities to be part of a market and may develop additional functionality (e.g. user interface, prompts etc) to compete with other solutions available on the market. As the solution has not been create specifically for a specific organisation and the locality it is unlikely to meet the exact needs of that organisation and the population served. The risk here is developing a 'drop in' solution creates is a mismatch between solution and local need. This results in gaps and duplications in capabilities which are different in different localities and creates more inefficiencies within the system (i.e. the solution doesn’t quite do what we want it to do).
Of course it is not as simple as having 'drop in' solutions, successful implementation of new solutions within a healthcare organisation means the healthcare organisation needs to change to absorb the innovation. The healthcare organisations need to flex, this means requiring changes in processes, roles, and training staff to ensure a new or modified skill set. The amount of change required in the healthcare organisation is different for each locality depending upon the local need. As this change management is resource intensive both in terms of time and money in addition to the complexity of the organisation and services in the locality it is unlikely that the locality will fully optimise around the new solution. Inefficiencies due to duplications and gaps between new solutions and current service provision persist.
We see solution providers are trying to overcome the key barriers to scale such as variation in populations, services and staff (roles and skills) across different localities. It is becoming more common to see solution providers better supporting localities to have more tailored solutions. Some provide change management support and semi-structured solutions which have elements of customisation to better suit the local needs.
One of the ramifications of this approach in addition to the inefficiencies is the healthcare organisation becomes optimised around the solution. This makes it more difficult for healthcare organisations to move to a different solution - the resources required can become a barrier to being able to shift and change solutions flexibly. Even with this approach in reality there will still be functionality duplication and gaps creating inefficiencies. Is there another way of solving this problem?
Top down or bottom up - more fragmention or less inefficiencies?
An alternative approach could be to support healthcare providers and localities to develop solutions based upon nationally agreed functionality and standards. For example, if the right collaborators are brought together can we enable clinical teams with healthcare professionals to work with software developers to co-develop digital based solutions that provide the nationally required functionality in a way which complements local needs? This moves the cost away from purchasing solutions to the development of solutions. However it also risks fragmenting the landscape as well as duplicating effort in each locality wasting resources. This might be mitigated through the use of standards, phased solution development and sharing across localities.
New opportunities to think differently
It was recently revealed that an anticipated NHS reform bill will potentially shake up the commissioning of health care services - currently amounting to £9 billion. In addition there may be Trust mergers and integrated care providers. These in combination create an opportunity to reconsider how standards, cross working and collaborative development could support locally developed solutions that share foundational infrastructure such as database, communications protocols etc while supporting localities to be able to tailor the solutions to meet the specific needs of the local population. This in theory could reduce the inefficiencies, there will always be a need to up skill staff and change processes but if developed with this approach the solutions will fit local needs more seamlessly creating less duplications and gaps which could potentially reduce inefficiencies.
We are seeing parts of this locality developed solutions approach emerging where organisations such as AT Medics, Haxby Group, Hurley Group and Here are developing internal solutions that are being made available to other regions and providers.
This is an opportune point in time as healthcare systems move to integrated care provision. We have an opportunity to modify how we develop and evolve healthcare systems facilitating locally developed solutions to complement scaled standard solutions, potentially reducing inefficiencies and improving care provision to each community.
Enjoyed this post? Get in touch Twitter or LinkedIn to share your thoughts!