Background
After several years of development ICBs were formally established in 2022, they started as STPs (Sustainability and Transformation Plans) in 2016 and eventually evolving into ICBs. However, from the beginning to today in 2025 they have had varied interpretations of their roles and responsibilities. Lord Darzi’s recent report identified this variation and recommended a more structured and strategic approach, providing much of the rationale for the changes now underway.
Redefining the role of ICBs
The revised ICB model narrows the role of ICBs and focusing on particular functions while incorporating strategic commissioning and collaborative leadership. However, the levers for change have shifted as ICBs will monitor and benchmark provider performance but the regions will be accountable for performance management – changing the ICB/provider relationship. Front and centre in the new model is a much stronger emphasis on using data and intelligence to predict, monitor, and shape healthcare delivery. ICBs are expected to lead on improving population health, reducing inequalities, and ensuring effective budget use.
A brief overview
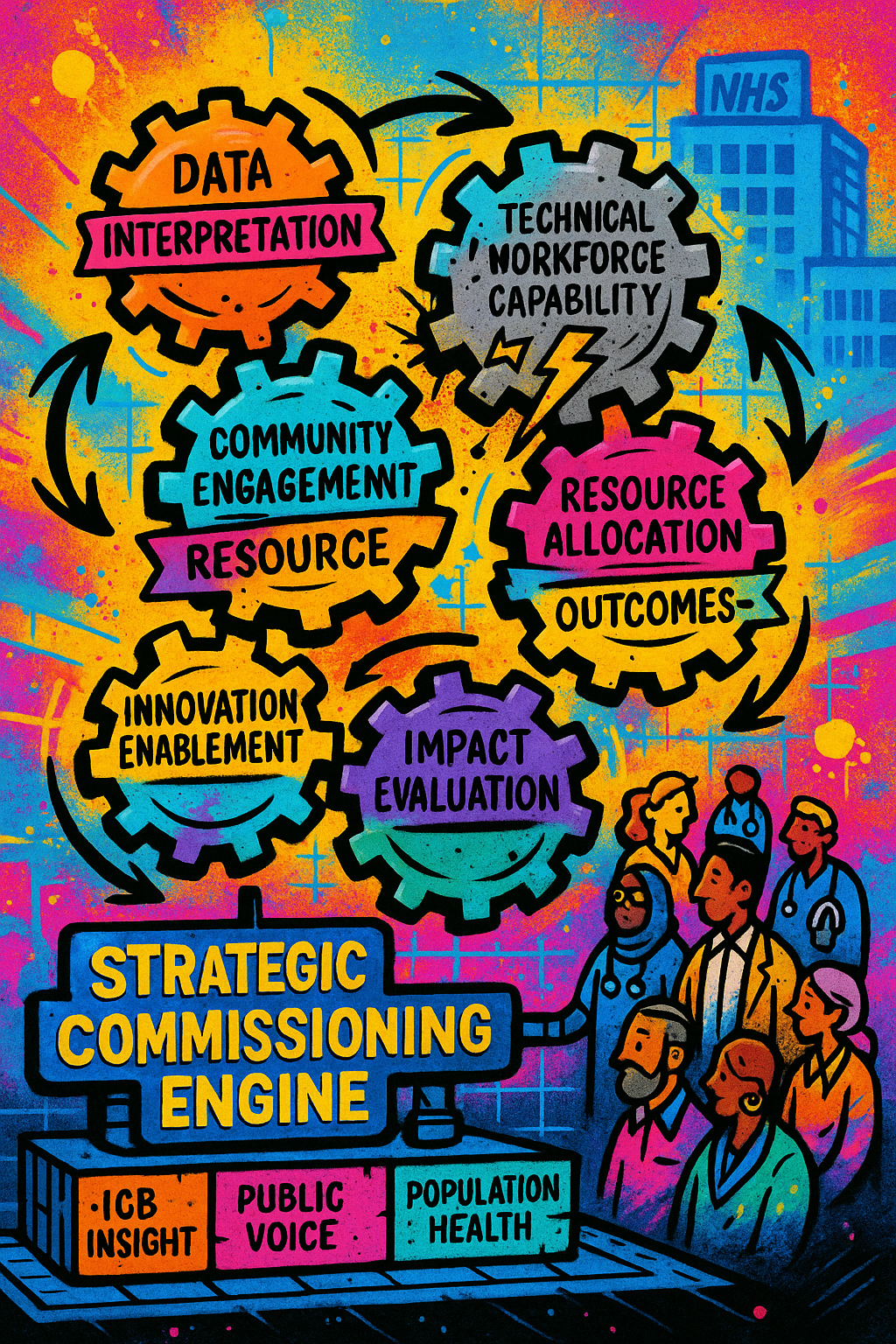
The new model outlines four core functions and capabilities:
- Understanding Local Context
ICBs are expected to have advanced data capabilities to interpret real-time information about health needs, service use, and system performance. This includes modelling demand, identifying care gaps, and forecasting future trends. Importantly, this isn’t just a technical task it involves convening stakeholders, understanding community expectations, and interpreting meaning from the data for the local context. - Strategic development with people
Long-term health strategies must be co-developed with people and communities, grounded in values-based decision-making, and informed by horizon scanning and data synthesis. There’s a clear shift toward aligning funding with need and impact, using measurable outcomes and metrics. - Strategic Delivery
ICBs are expected to use data to match resources with services and outcomes, use modelling of new provider configurations, and adopt innovative contracting mechanisms such as blended payments and shared savings. This will require agility and the ability to support innovation among providers and staff. Interesting to note here the potential for innovation through payment mechanisms for long-term change and innovation combined with the opportunity for ICBs to introduce new providers as we’ve seen with virtual wards. - Impact Evaluation
Monitoring day to day performance and evaluating the impact of commissioned services. Using a continuous process involving dashboards, benchmarking, and community co-design. This moves the system closer to a responsive system able to use data and adjust services dynamically – this is assuming contracts, capacity and capabilities allow for this to happen!

Shifting Responsibilities
The plan is to also redistribute responsibilities across the system:
- Kept by ICBs: Population health management, strategy development, quality management, governance, and organisational operations.
- Shifted to Regions: performance management, system coordination and emergency preparedness, strategic workforce planning including development, education and training.
- Shifted to Providers: sustainability plans, digital leadership and transformation, pathway and service development, estates and infrastructure.
- Shifted to Neighbourhoods: Primary care operations and transformation.
Key Challenges and Questions Ahead
There’s a significant amount of detail in the model document but there are many assumptions, challenges and questions remaining:
- Workforce Capability and Competition:
One of the most immediate barriers is the availability and salary costs of the skilled technical workforce required to implement the data and intelligence approaches the underpin the new model. Analytics, strategic commissioning, and system design are in high demand. There's a real risk that ICBs and providers will end up competing for the same limited pool of talent – provider competition for staff has happened previously. Without coordinated workforce planning, including investment in career pathways and skills development, the system could fragment rather than integrate. - Joined-Up Workforce Planning:
Workforce strategy is being shifted to regional and national levels, while the day-to-day reality of service transformation is shifting to providers. As new roles emerge and existing roles change through technological advancement, there must be a clear bridge between national workforce policy and local workforce planning to prevent misalignment between technology and staffing. - Public as shapers of services:
To work with the public in order to collaboratively develop services needs different skills, culture and competencies especially for engagement approaches like deliberative dialogue. Will this become a core competency for ICBs and how will they be supported to develop the capabilities or will it be left to source externally - Changing the Leadership Model:
Leadership capabilities need to shift significantly. ICB leaders must be comfortable with data interpretation, collaborative governance, and convening diverse stakeholders including meaningful public engagement. Is the current system investing enough in developing these system-wide leadership skills? - Automation, Operational Efficiency, and Fragmentation:
Many of the data-driven expectations placed on ICBs require automation of data collection, analysis, and reporting. Currently, much of this is still manual and labour-intensive. There are persistent issues with data standards, fragmentation of IT systems, and siloed datasets that need solving for data to be used and improved. Transformation and digital leadership is moving to the provider level relying on providers collaborating to adopt interoperable tools and platforms to break down data silos rather than reinforce them. - Transformation and Scaling:
As mentioned, tech transformation and leadership moves to providers as does service development. The risk is siloed transformation around organisations not people, can strategic commissioning and collaborative leadership negate this risk? Many ICBs have struggled to move the digital agenda forward so this might be more of a continuation of the current situation rather than a step back. One overlooked area is scaling, despite abundant innovation in the NHS, there is a struggle to scale successful pilots. The ICB model assumes that innovation can be identified, evaluated, and spread. Key questions remain: With technology and transformation leadership moving to providers, how does the ICB model support the desperately needed scaling? - Long term focus needs long term structures:
The ICB model envisions ICBs as strategic organisations with a long-term approach to improving population health. This requires stable structures over time. However, as we’re seeing now, shifts in governance and organisational form historically disrupt progress. For ICBs to maintain a long term focus, the system must preserve and support the structure itself and incentivise long term focus amongst dealing with everyday needs. The key question is whether ICBs can evolve over time rather than being replaced at the first sign of difficulty.
A System in Transition — and at a Crossroads
The ICB model suggests a more narrowly defined structure between regions and providers focused on population health, data-led insight, and decision-making with a long-term strategic focus. It also creates a requirement to involve people genuinely in shaping healthcare services. Historically, frequent structural reorganisations in the NHS undermine institutional memory, stall progress, and create fragmented digital systems. For ICBs to enable the system to have long term strategic focus means they need to themselves have stability. Addressing workforce, leadership, and technology gaps is critical for ICBs to meet these new expectations as data and insight centres using strategic commissioning and people's voices to address care needs. The budget cuts, abolition of NHS England, and new ICB model are shocks to the healthcare system. Will the system have the permission and freedom to not just survive but become antifragile – instead of absorbing pressure dynamically adapting and improving to become better.
Enjoyed this post? Do share with others! You can subscribe to receive posts directly via email.
Get in touch via Bluesky or LinkedIn.
Transparency on AI use: GenAI tools have been used to help draft and edit this publication and create the images. But all content, including validation, has been by the author.

