The NHS 10-Year Plan is due any day now. With so many snippets already trailed in the press, you might wonder whether anything in the final document can still surprise us. It’s definitely on my mind!
One question I’ve heard and seen regularly being asked is: why bother with another plan when today’s challenges of ageing population, widening inequalities, insufficient workforce and long waiting lists are hardly news? I’d suggest it’s because a published plan does more than list problems and actions: it signals priorities, aligns this with funding and metrics, gives local leaders the impetus to act and focuses efforts across NHS, industry, research, charities and other public sector bodies.
The last big “North Star” setting document was 2019’s Long Term Plan. It promised digitised outpatients, digital first services, patient empowerment, further development of the NHS App and more. Delivery got tangled up in COVID-19, but the ambition continued to determine the investment and healthcare activity. I'm sure most people have opinions on how successful that plan has turned out. But has healthcare truly transformed as the Long Term Plan envisaged? I'd say no, the NHS of 2019 is still visible albeit with technological progress in parts. Since 2019 there have been leaps in technology such as AI, better evidence base for other technologies like digital therapeutics and robotics while pressure and challenges have become more pressing. This all means a new plan is should help signal priorities, funding and focus. With all this in mind, here are three lenses I’ll use when the plan finally lands.
1 What have we learnt from what the NHS App already tells us
I built a quick dashboard using the data from the Office for National Statistics’ Opinions and Lifestyle Survey, focusing on the NHS App information. In England 66% of respondents use the NHS App, 32% don’t and 2% don’t know. Uptake among older age groups is better than many might assume, bucking tech adoption trends, this quiet success deserves greater celebration.
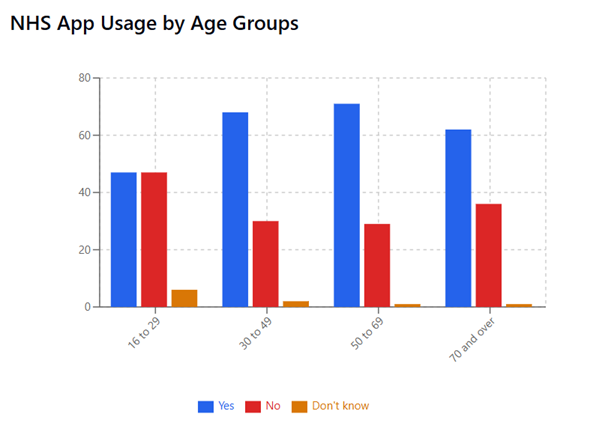
Yet 19 % of non-users are digitally excluded by skills, confidence or lack of kit. If the App is to become the AI-powered “digital front door” digital exclusion needs a far greater focus. The next figure of interest is another 15 % of non-users have never heard of the App - that surprised me! For those involved in healthcare and tech the NHS App can feel ever-present in headlines and comment pieces. However, it’s clear comms are missing a significant proportion of the public. Which means there needs to be changes in how the NHS communicates and engages with the public for greater reach through targeted messaging, staff who have the time and knowledge to walk people through the App and involvement of trusted community groups.
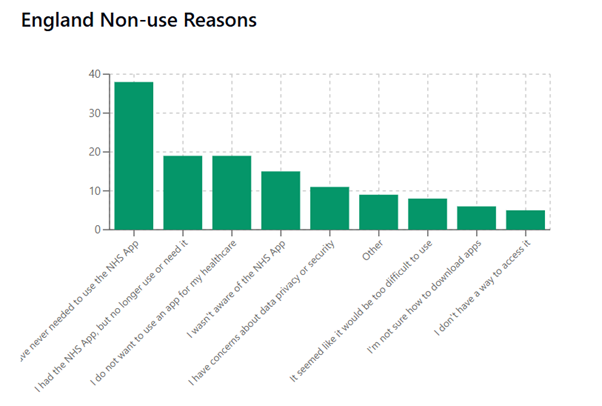
Finally to note, 11 % of those not using the NHS App worry about data security and privacy. Which leads us to the second lens...
2 Creating the right conditions for data sharing
Public deliberations over the past two years paint a consistent picture. People largely trust the NHS with data use but also expect the following:
- Security – modern use of technology for security combined with good staff training
- Transparency – related to comms once again is the expectation of better information on data initiatives including clarity on who has access to patient information for each initiative. The public also expect role based access and scenario based access, but not full patient information. Instead the public consistently expect staff to access information that is digitally curated to be relevant.
- Accountability – the public want clear structures, processes and sanctions for data use and misuse. Linked to transparency, the public would like the use of accessible audit trail on how their data is accessed and used in order to deter misuse.
- Patient choice – the public want to be informed on how their individual data is used and have the ability to choose how data is shared. Importantly there’s a need to acknowledge here that what is considered sensitive information can be highly individual.
Interestingly recent public deliberation concludes the data controllership model needs to change. You may be aware that GPs are data controllers which contributes towards the high trust in the NHS data use but this model also asks much of GP practices and staff including increased risk. Recent research shows that the public think the current model places too much burden on GPs and stretched practices with too little on national bodies when it comes to data use for secondary purposes. A revised model could preserve trust while delivering the consistency modern data flows demand.
So, alongside digital inclusion work and much deeper communications, how is data controllership, transparency and accountability changing to meet public expectations?

3 Avoiding technology overreach
It can be easy to be caught up in the promise of technology. However, we need to keep in mind that the limitations define the use and it’s the combination of technology with other approaches that often make dramatic change possible. There is an appealing myth that a reminder will suddenly drastically improve medication adherence, a single text will get everyone to screening or signposting to an app will make everyone change behaviour. In reality, tech is only ever part of the answer. Reminders matter, but so do travel links and costs, caring responsibilities and a numerous other considerations.
Harnessing technology therefore means investing not only in code but in people: analysts who translate dashboards into insight, clinicians who co-design pathways, staff who coach and shift behaviour, and leaders confident enough to retire tools that do not deliver. Behaviour change, service redesign and wrap-around support are the multipliers that turn clever software into better outcomes. Will the plan signal a greater focus on technical workforce development? Long needed and long overlooked!
So is there humility to embrace the limitations of technology and how are other non-technical techniques being brought into use to enable impactful transformation not creating shiny new veneers but tools that make complex care structures simple and effective.
Putting it all together
The 10 year plan will set a North Star for the NHS at a time of significant pressures and change. Technology is one of the three priorities for government. The NHS has years of experience in the use of technology and good engagement with the public which tell us there needs to be greater focus on digital exclusion, better communications, improvements to data accountability, trust and controllership as well as not over depending on tech but designing around the limitations. How will the plan learn from the past to inspire hope and change? Time will tell…
You made it to the end!
Hopefully that means you enjoyed this post, if so please share with others and subscribe to receive posts directly via email.
Get in touch via Bluesky or LinkedIn.
Transparency on AI use: GenAI tools have been used to help draft and edit this publication and create the images. But all content, including validation, has been by the author.

