If you enjoy this post please share to widen the discussion and consider subscribing for weekly articles to your inbox!
Many thanks to colleagues Sven Jungmann, Tim Conibear, Muir Gray and Anant Jani with who I had the opportunity to co-author the recently published paper "Using technology-enabled social prescriptions to disrupt healthcare". Below is a summary of the discussions within the article, the full paper can be read on the Journal of Royal Society of Medicine website or for those without the journal subscription you can free access the full text via Oxford Research Archive.
It is common knowledge healthcare systems are under pressure and that many patient conditions are lifestyle related and reversible:
Healthcare systems are facing increasing need and demand because of aging populations, increasing chronic disease and multimorbidity, and new therapeutics and diagnostics being brought to market. These factors, when combined, require unsustainable levels of funding. We must also acknowledge that a large proportion of chronic diseases that plague healthcare systems are preventable or can be brought into remission through lifestyle interventions and that 70% of health outcomes are determined by social factors that remain mostly unaddressed in healthcare systems predicated on the biomedical model.
There’s an increasing enthusiasm and interest in community activities (social prescribing) as an alternative means to help people maintain or improve wellbeing:
the rise of social prescriptions across European countries gives hope that there are non-biomedical means we can use to improve patient and population outcomes while optimising resource utilisation. Social prescriptions provide a way to connect individuals to sources of support within their community to address social determinants of health and encourage self-care for a variety of physical and mental health conditions.
Social prescribing has the potential to bend the healthcare resource requirements curve downwards or at least stop the upward trend:
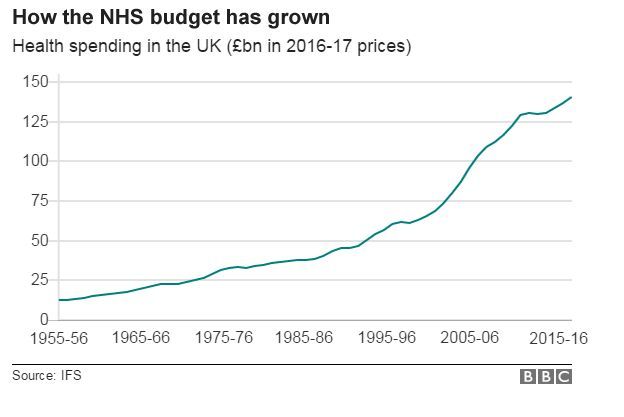
Social prescriptions have the potential to affect our health at much lower cost and fewer side effects than most medicines. Social prescriptions are poised to become a key disruptive force in 21st century healthcare because they can: a) be personalised and be highly adaptable to individual needs/expectations, which is currently largely impossible for most pharmaceuticals; b) effectively address many health and care issues associated with lifestyle-related chronic conditions; and c) address non-biomedical issues related to social determinants of health.
Why does tech have a unique role to play in realising the vision for social prescribing:
a) digital technologies make it easier and cheaper to obtain relevant information on individual patients, providers and the system; b) they can increase flexibility outside of the traditional place-based care approach (e.g. online remote monitoring of vulnerable people and flagging changes in conditions that might require medication adjustments); and c) they provide 24/7 interaction and automated functionality with the ability to provide nudges to patients and for the user to deliver frequent feedback as needed.
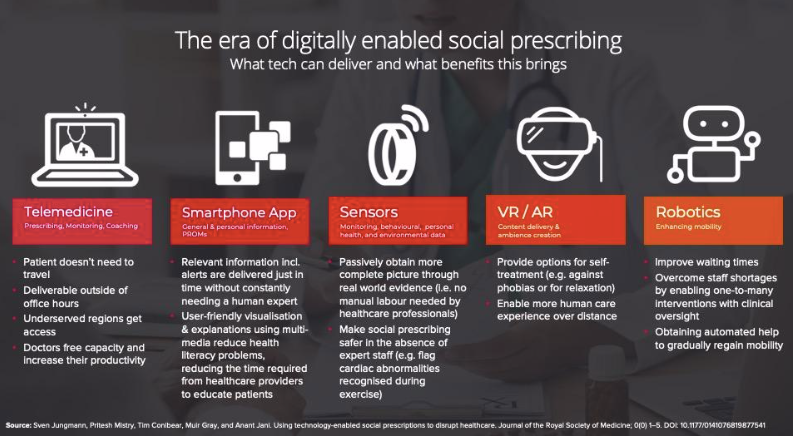
Tech enables reach:
tech-enabled social prescriptions have the potential to deliver services to those who never had access to them previously. This is particularly important in resource poor settings where tech-enabled social prescriptions could facilitate access to healthcare and also focus on lifestyle interventions to keep people healthy, rather than putting them at risk of developing preventable chronic diseases
Social prescribing is not a medical intervention rather it is helping individuals access to community based activity and support. Activity that can help an individual improve and so can be accessed by patients via healthcare professionals (or directly by the individual) to maintain or improve their wellbeing. If social prescribing is not a medical intervention then it doesn’t necessarily need to have the level of evaluation expected of a medical intervention but it does need to be quality assured with an appropriate level of rigour so patients with serious conditions are not exposed to an unnecessarily increase in risk. This is where digital can help to create trust and unlock data that can support quality assuring social prescribing for the multiple stakeholders to also mitigate any negative consequences.
Wearables and sensors can give information and insights that previously were not possible to collect. Through improved information flows and multiple measures of impact not only is it possible to capture the value of social prescribing but unintended consequences can also be monitored and mitigated through quality improvement approaches.
Digital has huge potential to unleash the use of social prescribing to support patients and people with medical conditions. It can democratise access, quality assure activities and provide insights to create impact information specific to each of the multiple stakeholders. Read the full paper on the JRSM website or free access here.
Enjoyed this post? Do share with others! You can subscribe to receive posts directly via email.
Get in touch via Twitter or LinkedIn.
Quick links to recent interesting articles:
- In 2019 poor healthcare IT security has cost $4B. There's increasing prevalence and cost of poor cyber security in healthcare.
- The digital divide is not just poor people who can’t afford a home but a combination of over surveillance and invisibility of the most deprived populations
You may also like: